55 years old male with pain in abdomen
Hi, I am Arefin Sadat, a final-year MBBS student. This is an E-Log that depicts the patient-centered approach to learning medicine. This E-Log has been created after taking consent from the patient and their relatives. The links that were used by me for understanding the available data on the particular disease have been mentioned below in each post. I hope you learn valuable information after giving it a good read.
PATIENT HISTORY: Pt is a 55 yr old male, doing business supplying small machine parts.
CHIEF COMPLAINT:
1) Pain in the rt quadrant of abd for the past 10 months.
2) c/o incomplete evacuation of bowel for the past 20 days
At the age of 12 yrs, he c/o anorexia, incomplete evacuation of stool, and acidity. He was taken to a local Dr. who detected hepatomegaly and prescribed medications, taking which resolved his symptoms within a few days.
At the age of 13, he c/o of high fever (103-104F), headache, and general body weakness lasting for 3-4 days, resolved with medications. 2 yrs later again it happened again.
In 2020, one day he went to an occasion, where in he ate a lot of fries, chicken, and sweets. After returning home at night, he started c/o localized intense pain in rt upper quadrant. The pain was increasing as the night progressed and taking medication for gas did not help. The next day his pain became unbearable and got admitted to a hospital, wherein he was injected with medication to relieve the pain. His pain reduced slowly. USG was gone which detected gallstone.
He went to a Dr. who did a laparoscopic cholecystectomy. He had no complaints after that.
In 2022, he c/o localized mild pain in upp. rt quadrant. Initially, the pain would occur at any time of the day 1-2 times daily, lasting for 10-15 mins. Then mostly after dinner when he went to sleep in a supine position. On tossing and turning to either side slowly the pain would disappear after 10-15 mins. For the past few wks, the pain happens 4-5 times a wk. Dr. prescribed paracetamol which reduced pain temporarily. Then USG and CT abd were done which revealed a liver abscess. Dr. performed USG-guided percutaneous drainage, but during a follow-up, Dr. told there had been not much improvement and he would need a laparoscopic drainage of liver abscess. He didn't do any further consultation.
The trend of the abscess size in the subsequent USG found that it was becoming smaller.
Pt reported for the past few months he is passing brown colored greasy stools.
For the past 15-20 days, he is experiencing incomplete evacuation of stool.
After being diagnosed with a liver abscess he lost 4-5 kgs of wt which he regained in the past few months.
On Feb 2023, secondary suturing was performed to remove the lung abscess. The possible reasons doctors figure out for his abscess that followed his cholecystectomy outside one year back is that the gall bladder perforation leading to the spillage of the gall stones ( as intra operative complication), which leads to formation of abscess in months.
Patient was adviced to take a protein powder.
After few days of operation, now his BP is 120/80, appetite normal, taking protein food, talking normally, sleep normal, motion normal, wound is healing fast. The patient is doing well. All natural activities appear to be normal.
Pt denied any history of HTN or DM.
ADDICTION: He started eating paan with tobacco in it at age of 17 yrs. Used to have 10-15 times daily. After being diagnosed with a liver abscess he eats 1-3 times daily.
FAMILY HISTORY:
Father - c/o loose motion, sudden urge to defecate, BPH
Mom - death due to stage 4 gallbladder Ca.
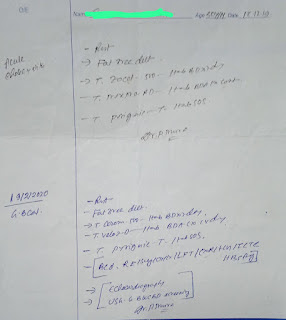
Clinical Picture:
Post operative follow-up:
According to the patients advocate the patient is doing well.
At first, from the wound site there was little discharge fluid which upon regular dressing, almost disappeared.
At present, the local doctor suggested a ointment to use on the wound site.






















Comments
Post a Comment